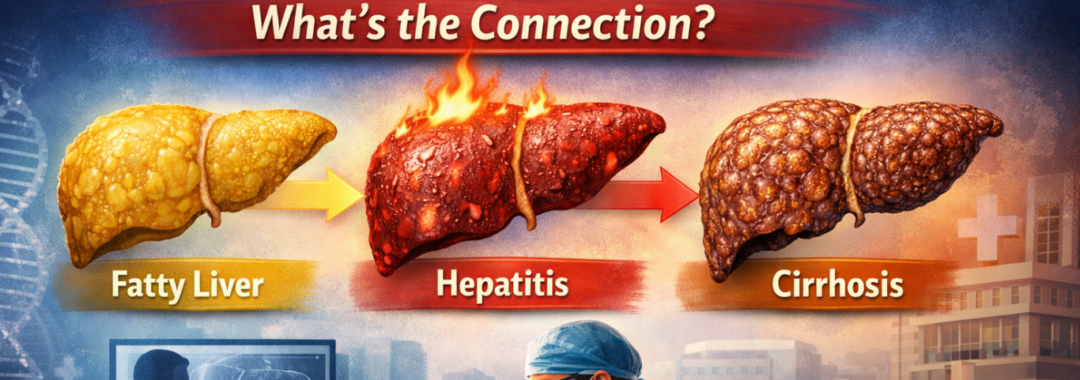
When someone hears the words fatty liver, hepatitis, or cirrhosis, it can feel overwhelming. Are they the same? Are they stages of one disease? Or are they completely different problems?
Let’s simplify this.
Think of your liver like a hardworking factory inside your body. It filters toxins, processes nutrients, helps digestion, stores energy, and supports immunity. Now imagine what happens when that factory slowly gets clogged, inflamed, and eventually scarred. That’s exactly how fatty liver, hepatitis, and cirrhosis are connected.
In this article, we’ll break everything down in simple language so you truly understand what’s happening inside your body—and when it becomes serious enough to need expert care, including consultation with the best liver transplant surgeon in India.
1. What Is Fatty Liver Disease?
The condition known as fatty liver occurs when fat is accumulated within the liver. A tiny percentage of excess fats is considered normal. However, if fat accounts for greater than 5- 10% liver’s weight, it can become problematic.
It’s similar to oil getting into the machine. Initially it’s not a problem, and the machine continues to function. However, over time it will slow down, and it may even break.
A lot of people suffering from fat livers don’t know they’re suffering. There may be no signs in the initial stage.
2. Types of Fatty Liver
Non-Alcoholic Fatty Liver Disease (NAFLD)
It is common in those who consume little or any alcohol at all. It is common among people who:
-
Obesity
-
Diabetes
-
High cholesterol
-
A lifestyle that is sedentary
Alcoholic Fatty Liver Disease
This is caused by heavy drinking of alcohol.
If liver fattiness is not treated, it could lead to inflammation, and that’s when hepatitis starts.
3. What Is Hepatitis?
Hepatitis simply refers to an inflammation in the liver.
Inflammation is the body’s way of resolving the injury. If it lasts for a prolonged period it causes damage to liver cells.
It’s as a fire that could be triggered in the factory we mentioned earlier. It may begin small, but if it is not managed, it could cause major damage.
4. Different Types of Hepatitis
Viral Hepatitis
-
Hepatitis A
-
Hepatitis B
-
Hepatitis C
As a result, Hepatitis B and C are major contributors to persistent liver diseases in India.
Alcoholic Hepatitis
Due to excessive drinking.
Non-Alcoholic Steatohepatitis (NASH)
This is a sophisticated form of fatty liver in which the buildup of fat can cause inflammation and even damage.
NASH is the most important link between fatty liver and cirrhosis.
5. What Is Cirrhosis?
Cirrhosis refers to an advanced form of scarring of the liver..
In the event of chronic inflammation for many years the healthy liver tissue gets transformed into scar tissue. Scar tissue doesn’t work like normal liver cells.
Imagine building walls to replace factory workers. There is space but there is no work to be done.
Cirrhosis can be serious and be life-threatening.
6. How Fatty Liver Leads to Hepatitis
Here’s how:
-
Fat accumulates in liver cells
-
Inflammation is caused by fat.
-
Inflammation damages liver cells
-
The damaged cells cause the condition of fibrosis (early scarring)
The term used to describe this stage is “NASH (Non-Alcoholic Steatohepatitis).
Not all people with fatty livers is likely to develop Hepatitis. However, if risk factors are uncontrolled, such as diabetes or obesity — the risk increases.
7. How Hepatitis Progresses to Cirrhosis
Chronic Hepatitis (lasting longer than 6 months) continually damages liver cells.
Over time:
-
Injuries that are repeated cause fibrosis
-
The fibrosis can cause severe scarring.
-
Liver structure becomes distorted
-
The blood flow through the liver becomes blocked
Then, it can lead to the development of cirrhosis.
This process can take anywhere from 10 to 20 years, but occasionally it can happen faster.
8. Common Symptoms at Each Stage
Fatty Liver
-
Often no symptoms
-
Mild fatigue
-
A little discomfort in the upper right abdomen
Hepatitis
-
Fatigue
-
Nausea
-
A loss of appetite
-
Eyes becoming yellow (jaundice)
Cirrhosis
-
Leg swelling
-
Abdominal fluid (ascites)
-
The cause of confusion (hepatic encephalopathy)
-
Easy bleeding
-
Very weak
When symptoms of cirrhosis show up, the damage may be advanced.
9. Who Is at Risk?
You could be at greater risk if:
-
Are you a diabetic?
-
Are overweight
-
Drink alcohol regularly
-
Are suffering from Hepatitis B (or C infection.
-
Are you a parent with a experience of liver disease?
-
Are you suffering from high cholesterol?
In India growing levels of diabetes and obesity are causing more cases of fatty liver quickly.
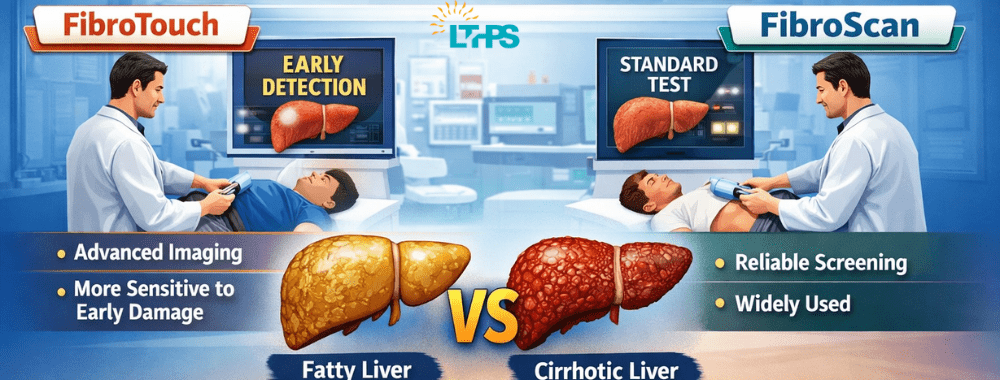
10. How Doctors Diagnose Liver Disease
Doctors make use of:
-
Tests for blood (Liver Functional Tests)
-
Ultrasound
-
FibroScan
-
CT scans or MRI
-
Liver biopsy (in specific cases)
A diagnosis early can make a big difference. The delay until symptoms show up could be risky.
11. Can Fatty Liver and Hepatitis Be Reversed?
This is the good news.
Fatty Liver – Yes, It Can Be Reversed
With:
-
Weight loss
-
Healthy diet
-
Exercise
-
Control of diabetes
-
Refrain from drinking the consumption of alcohol
Early Hepatitis – Sometimes Reversible
If inflammation is treated in the early stages the liver may recover.
Cirrhosis – Usually Not Reversible
After scarring has become severe the scarring cannot be completely reversed. But treatments can slow down the process.
This is why prompt action is crucial.
12. When Is a Liver Transplant Needed?
A liver transplant may be required at the time:
-
Liver is completely inoperable
-
In severe cases, complications from cirrhosis are common.
-
Liver cancer develops
-
Recurrent bleeding happens
At this point, medications alone are not enough to repair the damage.
The choice of the top surgery for a liver transplant in India is vital. Liver transplantation is a complicated procedure that requires expert knowledge, advanced hospital infrastructure and long-term follow-up treatment.
India is internationally recognized for its high-end liver transplant programs with high rate of success.
13. Importance of Choosing the Right Specialist
If the cirrhosis has reached its final stage you shouldn’t make a mistake.
An experienced team of liver transplant specialists can provide:
-
Proper evaluation
-
Living donor transplantation know-how
-
Monitoring post-surgery
-
Prevention of infection
-
Long-term survival care
When looking for the most effective liver transplant surgeon in India You should look for:
-
Experience with cases of high volume transplants
-
A strong hospital support system
-
Transparent patient communication
-
Proven long-term success rates
Make sure to consider this option, it could literally save the life of a person.
14. How to Protect Your Liver Today
You don’t have to be concerned about complicated steps.
Start by making it easy:
-
Maintain healthy weight
-
Exercise 30 minutes daily
-
Drink moderately or avoid alcohol.
-
Be vaccinated against Hepatitis B
-
Beware of injections that are unsafe
-
Control blood sugar levels
-
Consume a balanced and healthy diet
Think of your liver as an enduring friend who is working throughout the day. Shouldn’t it be treated with respect?
15. Final Thoughts
Hepatitis, Fatty Liver and cirrhosis aren’t distinct diseases. They often form as a part of a long chain reaction.
It is usually silent due to fat buildup. If ignored, it turns into inflammation. If the inflammation persists it can cause scarring. Advanced scarring may lead to liver failure.
The most important truth? Most of the cases are avoidable.
The early detection of the problem, changes in lifestyle and prompt medical attention can slow the process. If damage is more severe it is recommended to consult the most skilled liver transplant surgeons in India will ensure access to top-quality treatment and a better chance of survival.
Your liver is silent every day. The most you can try to do is to protect it, before it starts crying for assistance.
FAQs
1. Could fatty liver transform into cirrhosis?
Yes. If the fatty liver develops into the point of inflammation (NASH) and goes untreated for many years the condition can result in cirrhosis.
2. Does cirrhosis always result from alcohol?
No. Cirrhosis may result from an alcoholic liver condition as well as viral hepatitis, disorders of the immune system, as well as metabolic disorders, not just alcohol.
3. Can cirrhosis be treated without transplantation?
Advanced cirrhosis can’t be completely cure. Treatment is focused on reducing complications. In extreme cases liver transplantation is the only solution that can be permanent.
4. How long will the process take to cause hepatitis cause cirrhosis?
It could take anywhere from 10 to 20 years in chronic cases however, the timeframe varies based on the lifestyle, infection level, and the treatment.
5. What is the best time to consult an expert in liver transplantation?
If you are suffering from advanced symptoms of cirrhosis, such as abdomen fluid, persistent bleeding and confusion, or liver cancer, you must seek out a transplant expert immediately.