As the liver performs more than 500 essential functions, it is an organ that is essential to your overall health. These include the creation of vital proteins, processing blood, eliminating waste with bile, and filtering pollutants. You must take great care of it because it is your body’s natural detoxification system. You will learn some holistic approaches to a healthy liver:
It’s Best To Sweat
Your body must sweat. It will only do you a little good if you sweat while walking or because of the weather. Exercise causes your body to sweat, which has cleansing properties. If you haven’t been exercising, take up a regular exercise routine to help the toxins leave your body.
Exercises like yoga, running, working out at the gym, or even using a sauna can be beneficial. If you’re searching for easy ways to cleanse your liver, sweat is the best course of action. In case of serious liver failure issues, it is time to visit a liver transplant hospital.
Bid Farewell To Toxic Foods
Fast food is now considered to be the norm. Unknowingly, you eat many processed foods that are bad for the health of your liver.
Convenience meals, refined oils, and sugar deplete the body of vital nutrients and introduce additional poisons. Thus, if you’re wondering how to cleanse your liver, giving up processed food is a crucial dietary adjustment you should undertake. Swap these out for healthy, liver-
friendly options.
You Must Eat Foods Rich in Potassium
The human body requires the recommended daily allowance of 4,700 mg of potassium. Foods rich in potassium maintain a healthy cardiovascular system, assist in flushing the liver, and decrease cholesterol and systolic blood pressure. Foods high in potassium include bananas, beans, beet greens, spinach, sweet potatoes, and tomato sauces. Once you begin eating these foods regularly, you won’t need to worry about liver detoxification. These foods are very beneficial.
Wrapping it up:
The above approaches should be noted down to keep your liver healthy. You have to find the
best liver transplant hospital in India if you feel your liver’s health is out of time.
Author Archive: admin
Cadaveric Liver Transplant: What you need to know
Cadaveric Liver Transplant: What you need to know
Liver transplants are frequently performed using cadavers, or deceased donors, as a source of organs. The deceased donors gave their prior permission to donate their organs. A donor’s liver is removed and maintained for transplantation, which needs to happen within 24 hours of the donor being deemed legally dead (brain dead). The cadaveric donor programme aims to achieve maximum organ by harvesting from potential donors, including the liver, and provide easy access to transplant services.
What is Cadaveric Liver Transplant?
The procedure known as “cadaver donor liver transplantation” or “deceased donor liver transplantation” involves removing the liver from a brain-dead patient. A patient who is nearing the end of their liver failure receives a deceased donor liver transplant. Among the two liver transplantation techniques, cadaveric liver transplantation is one in which the deceased donor may have suffered a brain injury or been involved in an accident. What happens in a cadaveric liver transplant procedure?
A cerebral hemorrhage, head injury, or accident could possibly have affected the donor in a cadaveric liver transplant. Following the doctor’s official declaration of brain death, the organ is removed for donation with the family’s permission. A dead donor’s identity and the circumstances of their passing are kept private. The recipient’s waiting list position can always be discussed with the transplant coordinator and liver transplant surgeon.
A liver transplant from a deceased donor often requires four to fourteen hours of operation. The liver that was donated is transplanted after the injured liver is removed.
Post-operative care for cadaveric liver transplant procedure
After surgery, recipients will be closely watched in the intensive care unit (ICU) to ensure that their bodies are not rejecting their organs. Depending on the patient’s condition, they may be sent to the general ward. Testing for liver rejection helps to determine the probability of rejection. Immunosuppressants are given to patients to avoid rejection. There is also nutritional guidance and physiotherapy provided. Individuals who undergo cadaveric liver transplant surgery usually recover successfully. Approximately 90% of patients receive a liver transplant and survive for a minimum of a year, and many go on to live considerably longer. The total success rate is between 85 and 90%.
Final thoughts
The liver is an important organ in a body and is referred as human body’s powerhouse. It is the largest internal organ in the body which is situated beneath the diaphragm and above the stomach. Individuals who are suffering from end-stage liver illnesses or acute liver failure can benefit from cadaveric donor programme for liver transplants because these conditions may not be treated with therapy.
Best Liver Transplant Hospital in Delhi at Affordable Cost
In cases of severe liver illness, liver transplantation is a vital medical treatment that can save a patient’s life. The need for liver transplants is growing in India, especially in Delhi. At Liver Transplant International, one of the Best Liver Transplant Hospitals in Delhi, you can get treatment at an affordable cost.
Why Liver Transplant?
When a person experiences either acute (sudden) or chronic liver failure, a liver transplant can save lives. Acute Liver Failure (ALF) occurs unexpectedly, and there could be several causes for it. Hepatitis A and E acute viral infections are the most common cause in India. End-stage liver disease, another name for chronic liver failure, develops more slowly over several months, years, or even decades. The most common cause of chronic liver failure is cirrhosis, a disease in which the liver’s cells gradually die and are replaced with scar tissue throughout.
Advantages of Getting Treatment at Liver Transplant International
Here are some of the advantages you can get at Liver Transplant International, one of the Best
Liver Transplant Hospital in Delhi:
● Affordable Cost: One of the main considerations impacting the decision-making process of liver transplants is cost. Liver Transplant International is a more affordable option for people seeking high-quality healthcare.● Skilled Professionals: Liver Transplant International has one of the best and most accomplished medical experts, Dr. Neerav Goal, his expertise in liver transplant is well-known in India.
● Shorter Wait Times: Patients’ wait times for transplants are considerably shorter in Liver Transplant International.
● Modern Infrastructure: We have state-of-the-art equipment and modern amenities, ensuring a superior standard of treatment.
Why choose us?
Liver Transplant International is among the Best Liver Transplant Hospital in Delhi. We take a holistic approach with our multidisciplinary team to treat a wide range of liver conditions. A specialized facility in Liver Transplant International offers complete care and treatments related to liver transplants. At the helm of our liver transplant program is a team of highly skilled and experienced doctors who have overseen and nurtured the program’s growth from its inception.
3 Most common liver conditions in children
Liver which is one of the most important human body part, does more than 500 functions in the body. It generates the waste-carrying bile, breaks down fats in the small intestine, filters the blood to remove toxins, and transforms extra glucose into glycogen for storage. It also improves
the immune system by fending off infections. There are several liver conditions that affect children, and here, the three most common liver conditions in children are discussed:
What is the liver’s function?
As the second largest organ in the body, the liver, which is located in the abdominal cavity, does multiple functions:
● Generates bile, a chemical that helps in food digestion
● Stores excess nutrients
● Helps clear the bloodstream of impurities
● Regulate the levels of cholesterol and blood sugar
● Makes proteins that allow blood to clot normally, transport oxygen, and support the immune system.
What is a liver disease?
Anything that affects or reduces the liver’s ability to function is referred to as liver disease. It can occur as a result of an illness, bad habits or behaviors, or exposure to specific chemicals. It can also be acquired through family traits. If the liver is damaged beyond curing through treatment,
then getting the Best Liver Transplant would be the wise option. Different pediatric liver conditions
Here are three important pediatric liver conditions:
1. Portal hypertension: The spleen and intestine supply blood to the liver through the portal vein. Portal hypertension is the medical term for conditions that involve high blood pressure in these blood arteries or liver-related blood flow resistance. New blood vessels, known as collaterals, grow as a result of this pressure. The collaterals join the intestine’s blood flow to the main circulation, bypassing the liver in the process. So, impurities that were meant to be filtered by the liver find their way into the bloodstream.
2. Autoimmune hepatitis: A child’s own body causes autoimmune hepatitis. An autoimmune disorder is an attack on the body by the immune system, which fights disease. Here, there is an attack on the liver cells. Over time, this affects the liver by causing inflammation.
● Type 1: While it can start at any age, adolescence is the most common time for it to start (9 to 18 years old). Women and those with other autoimmune diseases like lupus, Crohn’s disease, or celiac disease are more likely to experience it.
● Type 2: In. It is more common in younger kids, particularly those with autoimmune disorders already.
3. Jaundice: Jaundice is caused by a rise in bilirubin in the body because of bile duct obstruction, liver cell abnormalities, or inflammation. It can occur as a result of the excessive destruction of a high concentration of red blood cells, which is common in neonates. The first and sometimes the only symptom of liver disease is jaundice.
Final thoughts Go to a reputable hospital as soon as possible if your child shows any of the symptoms or indicators of liver disease. Professionals there will correctly diagnose your child’s illness and start the best course of care. If there is a need for a liver transplant, then look for the Best Liver Transplant for a speedy recovery and rehabilitation.
Major Indications, When You Need A Liver Transplant!
Liver transplantation is necessary when the liver stops to function in the proper way. This could occur commonly because of acute failure from infections or complications arising from certain medications. Surgery of Liver transplant requires replacing a not functional liver with a healthy liver; where the healthy liver can be taken from either a deceased donor or donated by a living person.
What does a healthy liver performs?
The liver, body & largest internal organ, serves several vital functions, including:
Processing nutrients, medications, and hormones
Generating proteins necessary for blood clotting
Producing bile, crucial for absorbing fats, cholesterol, and fat-soluble vitamins
Regulating immune responses to prevent infection
In an ideal scenario, liver transplants are suggested for individuals facing serious complications due to advanced stages of chronic liver disease. In many other instances of abrupt failure in an otherwise healthy liver, transplant might also be an option.
More to consider before a Liver transplant:
The reason this procedure works is that the human liver has an incredible capacity to regenerate and quickly restore itself to its normal size following the surgical removal of a portion. As per a U.S., data in the year 2018, almost 8,200 liver transplants were conducted involving both adults and children. Among these, around 390 transplants utilized livers from living donors. Simultaneously, about 12,800 individuals were on the waiting list, anticipating a liver transplant.
Specific indications encompass various conditions such as:
Extrahepatic biliary atresia or hypoplasia Acute hepatic fulminant failure Additionally, other conditions such as Sclerosing cholangitis, Hepatic vein thrombosis (Budd- Chiari), Hepatocellular Carcinoma (HCC) at Stage I or II, or a single lesion, and various forms of cirrhosis including primary or secondary biliary cirrhosis, alcohol-related cirrhosis, chronic active hepatitis (A, B, C, non A, non B, autoimmune), cryptogenic cirrhosis, NASH-related cirrhosis, congenital biliary cirrhosis, viral cirrhosis, among others, are encompassed within this spectrum of liver-related disorders.
How does the transplant center performs?
Transplant centers house specialized Liver Transplant Programs designed to evaluate and treat these conditions. These programs offer comprehensive overviews, specific indications for transplantation, different types of transplants available, dedicated transplant teams, the transplantation process, discharge procedures, recovery plans, and specialized pediatric liver transplant programs. Additionally, some centers provide options for Living Donor Liver Transplant procedures.
Some more to understand: Liver transplant becomes necessary when the liver sustains significant damage, impairing its proper function. Key indications for a liver transplant comprise:
• Liver Failure: End-stage liver disease or failure resulting from chronic conditions such as cirrhosis, hepatitis, or genetic disorders.
• Chronic Liver Disease: Conditions like hepatitis B or C, autoimmune hepatitis, alcoholic liver disease, primary biliary cirrhosis, primary sclerosing cholangitis, and nonalcoholic fatty liver disease can lead to severe liver damage.
• Liver Cancer: Specific types of liver cancer confined to the liver may necessitate a transplant.
• Acute Liver Failure: Sudden and severe liver damage, often triggered by drug overdose, hepatitis, or other acute conditions, may urgently require transplantation.
• Genetic Disorders: Inherited liver conditions like hemochromatosis, Wilson & disease, or alpha-1 antitrypsin deficiency can cause liver damage, potentially requiring a transplant.
• Recurrent Liver Failure: In instances where a previously transplanted liver is failing or being rejected, another transplant might become necessary.
Final Words-
Need a liver transplant – considering factors discussed here in the blog. First most important is the patient & general health, and then next is the extent of liver disease. Next is availability of the donor. Evaluation at a transplant center involves thorough testing and assessment to determine if
transplantation is the most suitable path forward. Do get consultation at a proper time to deal with it.
What diet one should follow after a liver transplant?
Managing your diet and nutrition post-liver transplant is very important aspect. The diet maintenance is helpful in preventing excessive weight gain, and avoiding further any complications. It is also very important to ward off high blood pressure, infections, and other potential issues. The advice from the nutrition specialist or the treatment team will strictly be considered and followed that are tailored to your individual needs and lifestyle. Patients who’ve undergone liver transplants significantly enhance their long-term treatment success by diligently adhering to the rehabilitation program, with diet playing a pivotal role. This isn’t complex knowledge—maintaining a well-balanced diet is essential for anyone seeking a healthy life, let alone patients post-transplantation.
Role of the treatment team after liver transplant: Your treatment team is there to provide comprehensive care, integrating nutritional planning into the recovery process for transplant patients. Nutritionists play a crucial role in designing tailored dietary plans. We have discovered that the crux of post-liver transplantation well-being lies in adopting a nourishing diet. Here’s the key to achieving it:
Calcium: Enhancing bone strength becomes vital due to the risk of fractures and osteoporosis resulting from prednisone intake, a medication common among liver transplantation patients. Whey protein and certain leafy vegetables serve as rich sources of calcium. Additionally, nuts like almonds and seeds store substantial amounts of this essential mineral.
Fiber: The advantages of fiber are manifold, notably in maintaining a healthy weight. Fresh fruits and vegetables boast abundant fiber content, especially when consumed whole for optimal nourishment. Whole-grain wheat products, such as pasta and cereals, stand out as high-fiber foods offering significant health benefits.
Fats: Elevated levels of bad cholesterol pose added health risks and can hinder recovery. Conversely, integrating healthy fats into your diet contributes to overall health benefits. Opt for cold-water fish like tuna, abundant in omega-3 fatty acids, a remarkable element for promoting well-being. Vegetable oils and nuts serve as excellent sources of healthy fats too.
Vitamin D: Counteracting bone loss induced by prednisone intake involves incorporating Vitamin D into your diet. Dairy products, fresh orange juice, and fatty fish serve as excellent sources of this essential vitamin.
Protein: A crucial aspect of the rehabilitation program following a liver transplant, recommended by seasoned professionals in advanced medical centers like Delhi or Mumbai, involves allocating one-fourth of your diet to protein for at least two months post-transplant. Ensuring long-term
health benefits necessitates integrating protein into both your meals and beverages. People who prefer non-vegetarian food may choose for chicken, fish, eggs and lean meats, satisfying their dietary needs. Even people who eat vegetarian food also can opt from lentils, legumes, and dairy products, and also for vegan diet people, soy milk acts as a rich protein source. Additionally, nuts, seeds, and incorporating low-fat dairy products can assist in managing weight gain.
Guidance from your dietitian may encompass:
● Try having at least fruits and vegetables every day in five servings.
● Make an inclusion of poultry, lean meats, and fish in your diet.
● Ensuring an adequate daily intake of dietary fiber.
● Incorporating whole-grain breads, cereals, and other grains into your meals.
● Adhering to a low-sodium and low-fat diet.
● Choosing low-fat milk or other dairy products to support calcium levels.
● Following recommended food safety guidelines.
● Staying well-hydrated by consuming sufficient water and other fluids daily.
● Abstaining from alcohol consumption.
● Avoiding grapefruit and grapefruit juice due to their impact on a category of immunosuppressive medications known as calcineurin inhibitors.
Incorporating these elements into your daily dietary intake proves beneficial. Managing sugar
levels aids in regulating blood sugar. Adhering to dietary guidelines that exclude potassium (if
advised by your doctor) is crucial to avoid associated side effects and complications.
Avail the Best Treatment of Liver Transplant in New Delhi
Liver Transplant is a very crucial process and the success of any liver transplant mainly dependable on the experience and expertise of the team taking care of the transplant, including the surgeons, anesthesiologists, hepatologists, and nurses. Research the qualifications and experience of the medical professionals involved in the transplant program.
Know your surgeon:
Neerav Goyal – Head – DNB (Surgery) DNB (G.I. Surgery), MNAMS
He is holding specialization in Liver Transplants and Gastrointestinal Surgery and he is an experienced surgeon with various awards in liver transplant surgery. He has only one aim that he always delivers the best outcome to the patients with best consultancy options. He carries an experience of performing more than 2500+ liver transplants successfully.
What is the importance of liver?
The liver has captured its position under the body’s most vital organs, essential for sustaining life. Its multifaceted role encompasses crucial functions such as metabolizing substances, eliminating waste products, and synthesizing enzymes and proteins.
Who shall be considered themselves for liver transplant?
Only individuals whose liver disease has gotten so bad that their overall health is in danger should be considered for a liver transplant. These individuals typically have either developed liver cancer along with other conditions or have exhausted all available therapeutic options. The waiting period for cadaveric transplants can vary greatly, and some patients may pass away in the meantime before receiving a donor’s liver. Moreover, because living donor liver transplantation is a planned procedure, it can be performed only when a person truly requires it and when everyone on the team is accessible.
What we manage?
At our centre, we provide comprehensive treatment, care, and amenities for the liver and biliary system.
Liver failure: When the liver begins to fail, either from acute liver failure or cirrhosis, the illness is known as liver failure. Liver function is a rare condition that has to be treated right away.
Hepatitis: Hepatitis is an infection that results in liver inflammation. It may manifest in several forms, such as
autoimmune illness, alcohol- or non-alcoholic-induced fatty liver, hepatitis b, or hepatitis c.
Hepatocellular: Individuals with chronic liver disorders, including acute liver failure, are frequently detected with hepatocellular carcinoma.
Liver metastases: One type of secondary liver cancer is hepatic metastasis, which begins in another area of the body and
gradually moves into the liver. The malignant cells that begin to grow in the individual’s breast, liver, and any other region of their body are transported there and eventually settle to create another tumor.
Bile duct cancer: A condition termed cholangiocarcinoma, or bile duct cancer, arises in the bile ducts, which are tubes
that join the liver and gall bladder. The digesting liquid bile, a waste byproduct of the liver, is transported by the bile ducts. For the best liver transplant and to avail the best treatment of liver transplant in New Delhi, we are known as the greatest liver transplant doctor. We work with a group of other medical professionals at the liver transplant clinic in New Delhi to offer patients cutting-edge medical care.
How to take care of your Liver after Transplantation?
The liver transplant has emerged as a cutting-edge therapy for those with severe liver failure or end-stage liver disease. While replacing a diseased liver with a healthy liver is a successful method to cure liver disease, proper post-operative care is just as crucial to avoid graft rejection, infection after the transplant, and disease progression.
The following measures should be adopted as soon as you are released from the hospital following an effective liver transplant if you want a positive long-term outcome.
Ways to take care of oneself following a liver transplant
You must maintain the best level of fitness and health possible to ensure that the transplant will function for as long as possible. You must also receive ongoing treatment for your transplanted liver.
Skip the alcohol
If you had a liver transplant because of an illness caused by alcohol, you shouldn’t drink alcohol again because doing so could damage your new liver. This holds regardless of whether alcohol was not the primary cause of your liver disease but was deemed to have had a role in it. The rate of liver damage from alcohol after liver transplant is much more rapid than before transplant.
Clean environments
The first step towards successful rehabilitation starts at home. The family member should make sure the dwelling has appropriate ventilation when the patient returns home following a liver transplant. In the first three months after surgery, the patient must wear a mask when entering crowded areas. Practice cleaning your hands after speaking to strangers. The patient should have access to a unique towel.
Nutrition and diet
The patient will have a ravenous appetite after the procedure, which is really a positive sign. The patient must consume a diet high in protein. Water used for drinking needs to be secure, and tap water shouldn’t be consumed without at-home filtration. Salads and raw foods must be ignored. Additionally, one must avoid foods like sweets that could raise blood sugar levels. Often, post-transplant medications will cause blood sugar levels to rise, necessitating the usage of insulin for the first three months. You shouldn’t drink alcohol. Certain fruits which can drive the serum potassium levels up like banana, guava, coconut etc should be taken with caution in the first few months after transplant, since the CNI drugs being used as immunosuppression can increase the serum potassium levels.
Stay away from somebody who has an infectious disease
People who have had liver transplants must refrain from socializing with a lot of visitors since those who are ill can pose a threat and contaminate the patient. Therefore, do not let anybody with the flu, chicken pox, or measles into the room where the individual with the liver transplantation is resting.
Keep pets out of the house.
A liver transplant recipient must prevent interaction with animals. Some pets’ vomit, feces, bird droppings, and urine are contagious and can give individuals with weakened immune systems serious fungal diseases. As a result, it is best to avoid contact with animals to lower the chance of infection.
Adhere to directions
People who have had liver transplants must adhere to the recommendations made by the physician at the time of hospital release. You must refrain from performing strenuous exercises and lifting large objects. It is advised to get up and move around the house and locality, and performing regular tasks might hasten recuperation. Wait until your doctor instructs you to drive a car.
Everything you need to know about Fatty Liver and its type
The storing of excess fat in the liver results in the prevalent illness known as fatty liver disease. The majority of folks show no symptoms, and they don’t have any major issues. However, it occasionally can result in liver damage. The good news is that lifestyle adjustments may frequently prevent or even correct fatty liver disease.
Why does fatty liver disease occur?
Extra fat is formed in the livers cells and accumulates there in fatty liver disease. There are a number of factors that might be the cause of this fat gain. Alcohol abuse can result in AFLD. Heavy alcohol use can change several of the liver’s metabolic functions. Many of these metabolic byproducts have the potential to interact with fatty acids to create certain forms of fat that can build up in the liver. The etiology of fatty liver disease in those who don’t use a great deal of alcohol is poorly understood.
The several forms of fatty liver disease
Alcoholic and nonalcoholic fatty liver diseases are the two primary varieties.
1. Metabolic-associated fatty liver disease (MAFLD)
Metabolic-associated fatty liver disease (MAFLD) is the name for presence of hepatic steatosis the livers of light drinkers. MAFLD may be diagnosed if you have excessive fat in your liver and have no past of drinking heavily. Simple MAFLD is the name given to the disorder if there are no swelling or other problems.
2. Alcoholic fatty liver disease (AFLD)
Abundant alcohol use harms the liver. The initial stage of alcohol-related liver damage is known as AFLD. Simple alcoholic fatty liver is the name of the disorder if there are no swelling or other problems.
3. Acute fatty liver of pregnancy (AFLP)
When too much fat accumulates in the liver during pregnancy, it is known as AFLP. It’s a dangerous pregnancy issue that is uncommon. Genetics may have a role, albeit the precise cause is uncertain. AFLP often happens during the third trimester of pregnancy. It poses significant health concerns to the mother and child if left unchecked.
Causes of Fatty Liver:
For NAFLD: Insulin resistance, obesity, type 2 diabetes, high cholesterol, high blood pressure, frequent weight loss, and a lazy lifestyle. For AFLD: High level of alcohol consumption from very long time.
Symptoms:
● May not have noticeable symptoms in the early stages.
● With the disease progression, abdominal discomfort, fatigue, and jaundice may occur or felt.
What one should take care of to prevent himself from this disease?
● A build-up or depositing of fats in the liver.
● If one has a hereditary obesity, take care.
● High level of alcohol intake
● A high-fat diet
Diagnosis:
● Ultrasound
● CT scans, or MRI
● Liver function tests and blood tests
● Liver biopsy – it’s the most promising diagnosis.
Fatty liver can harm many organs in our body and hence may lead to some severe complications. One should avoid all such above elaborated risk factors. Fatty liver disease is a significant concern disease and a regular medical check-ups, healthy lifestyle, and early intervention can manage and prevent the conditions.
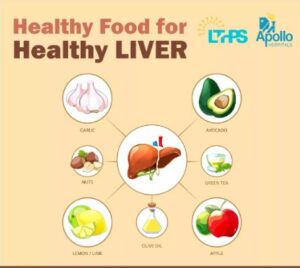
How Eating Healthy Food Affects Your Liver Health?
A popular quote mentions that “Let food be thy medicine, thy medicine shall be thy food.” This saying is actually producing the facts because food is the best medicine for a healthy mind, body and soul. A strong and good health requires healthy food that includes a balanced diet. so, to acquire a good health there is a simple formula that says eat what you actually don’t want or that don’t appeal you because a healthy food is a bank account that stores all healthy things for you.
To keep you liver in good health, it requires a nutritious and balanced diet. You liver is a crucial organ for processing nutrients and filtering hazardous compounds from the blood. To keep your liver working properly, you need to take care of your health. Read this blog to know more about how eating healthy food affects our liver functioning.
Why should we have a healthy diet?
Our body absorbs food nutrients such as carbs, fat, and protein into the bloodstream. These nutrients are taken to the liver, which metabolizes them before storing or using them to support critical physiological operations.
Furthermore, the liver cleanses potentially toxic compounds. Liver also purifies any potential toxin from our body
A well-balanced diet, commonly characterized as low in sugar and fat and high in fiber.
Selecting a diet from diverse foods is critical to ensuring the body receives all needed nutrients. Below are some of the food to avoid and eat to maintain your liver health.
What must be avoided to keep the liver healthy?
Fried/fast foods are heavy in fat and sugar and harm liver function. Furthermore, eating high-salt foods can cause fluid buildup and inflammation in the liver.
In severe liver injury, the organ cannot digest proteins effectively, resulting in a buildup of harmful byproducts in the blood. Reducing protein and boosting carbohydrate intake may be advantageous in such circumstances.
Because the liver is the primary organ for alcohol detoxification, limiting or restricting the intake of alcohol to one drink per day for women and two drinks per day for men can help to prevent liver damage.
Coffee can help reduce abnormal liver enzymes.
Coffee daily may help prevent your liver against MAFLD. Caffeine appears to reduce the amount of aberrant liver enzymes in persons who are predisposed to liver disease.
Vegetables to prevent fat accumulation
Compounds present in spinach and various other leafy greens may aid in treating fatty liver disease. This could be because cooking spinach (and other leafy greens) may lower polyphenolic content and antioxidant activity.
Reduce your sugar consumption
Sugar is bad for your overall health and liver. This sugar will be changed into fat, harming your body. In the future, you could develop fatty liver disease. So, do your liver justice and limit your intake of sweets to once a week.
Green tea
It’s loaded with catechins, an antioxidant. According to Research, it could protect against certain types of cancer, particularly liver cancer. You’ll get additional catechins if you make your tea and drink it warm. Iced and ready-to-drink has substantially lower amounts.
Grapefruit
Grapefruit provides antioxidants that support the liver. Grapefruit has two major antioxidants: naringenin and naringin.
Grapefruit is recognized to have two defensive effects: decreasing inflammation and preserving cells.
Fish can help lower inflammation and fat levels.
Omega-3 fatty acids are rich in fatty fish like salmon, sardines, tuna, and trout. According to Research, omega-3 supplementation may benefit patients with MAFLD by decreasing liver fat, increasing beneficial HDL cholesterol, and reducing the amount of triglycerides.
Additional treatment options for fatty liver disease
In addition to altering your food, the following lifestyle modifications can help strengthen your liver health:
- Get moving. Exercise and a healthy diet may assist you to lose weight while controlling your liver illness. Aim for thirty minutes of aerobic activity.
- Lower lipid levels in the blood. Reduce your saturated fat and sugar intake to help maintain your cholesterol levels in check. If eating and exercising aren’t cutting it, talk to your healthcare provider about medication.
- Maintain diabetes control. Diabetes and fatty liver diseases are frequently found together. Both disorders can be managed with diet and exercise. If your blood sugar level remains high, a doctor may give medications to bring it down.
Conclusion
If you’re suffering from MAFLD, some lifestyle and nutritional changes may reduce the risk of causing severe damage. The best thing is to improve liver function, minimize illness risk, and support healthy weight managment is to eat a well-balanced, nutritional diet high in proteins, fiber, and good fats.
If you have MAFLD or are concerned that you might have it, consult with a trusted healthcare provider to develop a treatment plan involving dietary adjustments and lifestyle improvements.