Alcoholic Fatty Liver Disease (AFLD) is one of those silent conditions that quietly builds inside your body—often without any major warning signs. If you’ve ever wondered what really happens in your liver after years of drinking, you’re not alone. Think of your liver as the hardworking “filter” of your body. When alcohol enters your system too often or in large amounts, this filter becomes clogged, strained, and eventually damaged.
In this article, we’ll walk through what happens inside your liver, why fatty liver develops, how it progresses, and when it becomes life-threatening.
1. Understanding Alcoholic Fatty Liver Disease
Alcoholic Fatty Liver Disease is the earliest and most common stage of alcohol-related liver damage. When you drink regularly, the liver starts storing fat because it can’t break down alcohol and fats together efficiently.
Imagine trying to clean your house while someone keeps throwing trash inside– it becomes impossible to keep up. That’s exactly what happens inside your liver.
2. How Your Liver Normally Works
Your liver is an incredible organ with over 500 essential functions. Here are some of the most important ones:
Filtering toxins from your blood
Processing fats, sugars, and proteins
Helping with digestion through bile production
Storing vitamins and minerals
Supporting immunity
Normally, it works quietly in the background without any complaints– until alcohol overloads it.
3. What Alcohol Does to Your Liver
Alcohol is treated like a toxin. The liver prioritizes breaking it down, ignoring other important tasks. When this happens repeatedly:
Fat starts accumulating
Inflammation begins
Liver cells become damaged
Scar tissue forms
Over time, the liver becomes less efficient, weaker, and unable to repair itself.
4. Stages of Alcohol-Related Liver Damage
There are three major stages:
a) Alcoholic Fatty Liver (Simple Steatosis).
This is the earliest stage. Fat builds up, but the damage is still reversible if drinking stops.
b) Alcoholic Hepatitis.
Liver cells become inflamed and start dying. Symptoms appear here.
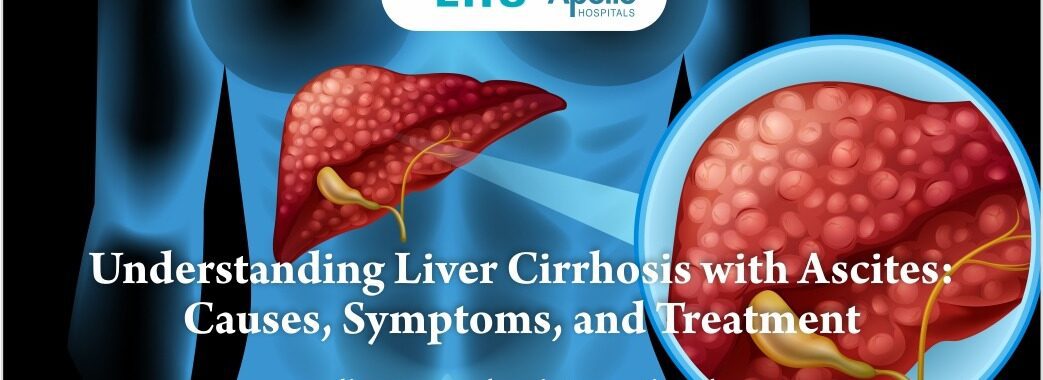
c) Cirrhosis.
Permanent scarring of the liver. This stage is dangerous and can lead to liver failure.
Skipping treatment can turn a mild condition into a life-threatening one.
5. Early Signs and Symptoms You Shouldn’t Ignore.
Alcoholic fatty liver is often silent, but some people develop the following:.
Constant tiredness.
Pain or heaviness in the upper right abdomen.
Loss of appetite.
Nausea.
Unexplained weakness.
Weight loss.
Yellowing of eyes (a later sign).
If you notice these signs– especially along with regular alcohol intake– it’s important to get evaluated.
6. Why Some Drinkers Develop AFLD Faster Than Others.
Not everyone who drinks develops fatty liver at the same speed. Several factors matter:.
Genetics.
Gender (women are more sensitive to alcohol-related liver damage).
Poor nutrition.
Being overweight.
Drinking patterns (binge vs daily drinking).
Some people may develop damage even with moderate drinking.
7. The Silent Danger: Inflammation Inside Your Liver.
Fat in the liver is not the only problem– it’s the inflammation it triggers. When liver cells become inflamed:.
They swell.
They stop functioning properly.
They release chemical signals that damage surrounding cells.
The immune system attacks these unhealthy cells.
Scar tissue begins to form.
Inflammation is a major turning point that shifts fatty liver toward more dangerous stages.
8. Progression to Hepatitis and Cirrhosis.
If drinking continues:.
Alcoholic Hepatitis.
Symptoms may include:.
Fever.
Vomiting.
Jaundice.
Abdominal swelling.
This stage is serious and requires immediate care.
Cirrhosis.
The liver becomes hardened due to scar tissue. At this point:.
Many liver functions fail.
Blood flow through the liver becomes blocked.
Toxins build up.
Liver cancer risk increases.
Transplant may be the only option.
This is why early detection is crucial.
9. Alcoholic Liver Disease vs Non-Alcoholic Fatty Liver.
Both conditions cause fat buildup, but their causes differ:.
Alcoholic Fatty Liver → due to chronic alcohol intake.
Non-Alcoholic Fatty Liver → due to obesity, diabetes, poor diet, genetics.
Symptoms and complications are similar, but treatment differs based on the cause.
10. Can Fatty Liver Be Reversed?
Yes– the earliest stage is fully reversible.
If alcohol is stopped completely:.
Fat reduces in weeks.
Inflammation settles.
Liver cells start regenerating.
Energy levels improve.
Overall health rebounds.
The liver is one of the few organs capable of repairing itself– but only if the damage hasn’t gone too far.
11. How Long the Liver Takes to Heal After Alcohol.
Healing time varies:.
2– 4 weeks: Fat begins to reduce.
3 months: Inflammation decreases.
6– 12 months: Many liver functions return to normal.
Cirrhosis: Damage is permanent and can not fully heal.
Complete abstinence is the most powerful treatment.
12. Tests and Diagnoses Doctors Use.
To confirm alcoholic fatty liver, doctors may recommend:.
Liver function tests (LFTs).
Ultrasound.
FibroScan.
CT scan or MRI.
Liver biopsy (in unclear cases).
Early diagnosis helps prevent complications.
13. Lifestyle Changes That Can Save Your Liver.
Here’s what you can do:.
a) Stop Drinking Completely.
Even small amounts can worsen fatty liver.
b) Eat a Nutritious Diet.
Include:.
Lean proteins.
Whole grains.
Nuts.
Fruits and vegetables.
c) Stay Physically Active.
Exercise helps burn liver fat.
d) Maintain Healthy Weight.
Obesity increases inflammation.
e) Stay Hydrated.
Water helps liver detoxification.
Small changes today can protect your liver for a lifetime.
14. When to See a Liver Specialist.
If you have:.
Persistent fatigue.
Abdominal pain.
Yellowing of skin.
Heavy alcohol intake.
Abnormal liver tests.
… it’s time to consult a hepatologist (liver specialist).
Finding the right specialist early can prevent long-term damage.
15. Liver Transplant: When It Becomes the Only Option.
If cirrhosis advances or your liver stops functioning, transplantation may be required.
A liver transplant can:.
Save your life.
Replace a severely damaged liver.
Restore normal functioning.
Improve quality of life.
If you’re searching for treatment options, consulting the best liver transplant surgeon in India is crucial for timely decisions and successful outcomes.
Conclusion.
Alcoholic Fatty Liver Disease is not just a “drinker’s problem.” It’s a silent condition that quietly damages your liver over years. The good news? It is completely reversible in the early stages. All it takes is awareness, early diagnosis, and lifestyle changes.
Your liver works tirelessly for you– give it the care it deserves. And if you or someone you know has progressed to a serious stage, seeking expert guidance from the best liver transplant surgeon in India could be life-saving.
Frequently Asked Questions.
1. Is alcoholic fatty liver disease reversible?
Yes. If alcohol is stopped early, the liver can heal completely within weeks to months.
2. How long does it take for fatty liver to develop after drinking?
It can begin after a few weeks of heavy drinking but worsens over years.
3. What are the warning signs of advanced alcoholic liver disease?
Jaundice, swelling, vomiting blood, confusion, and weight loss.
4. Can fatty liver turn into liver cancer?
Yes, especially if it progresses to cirrhosis.
5. When should someone see the best liver transplant surgeon in India?
If liver failure, cirrhosis, or complications like recurrent jaundice appear, early consultation is essential.