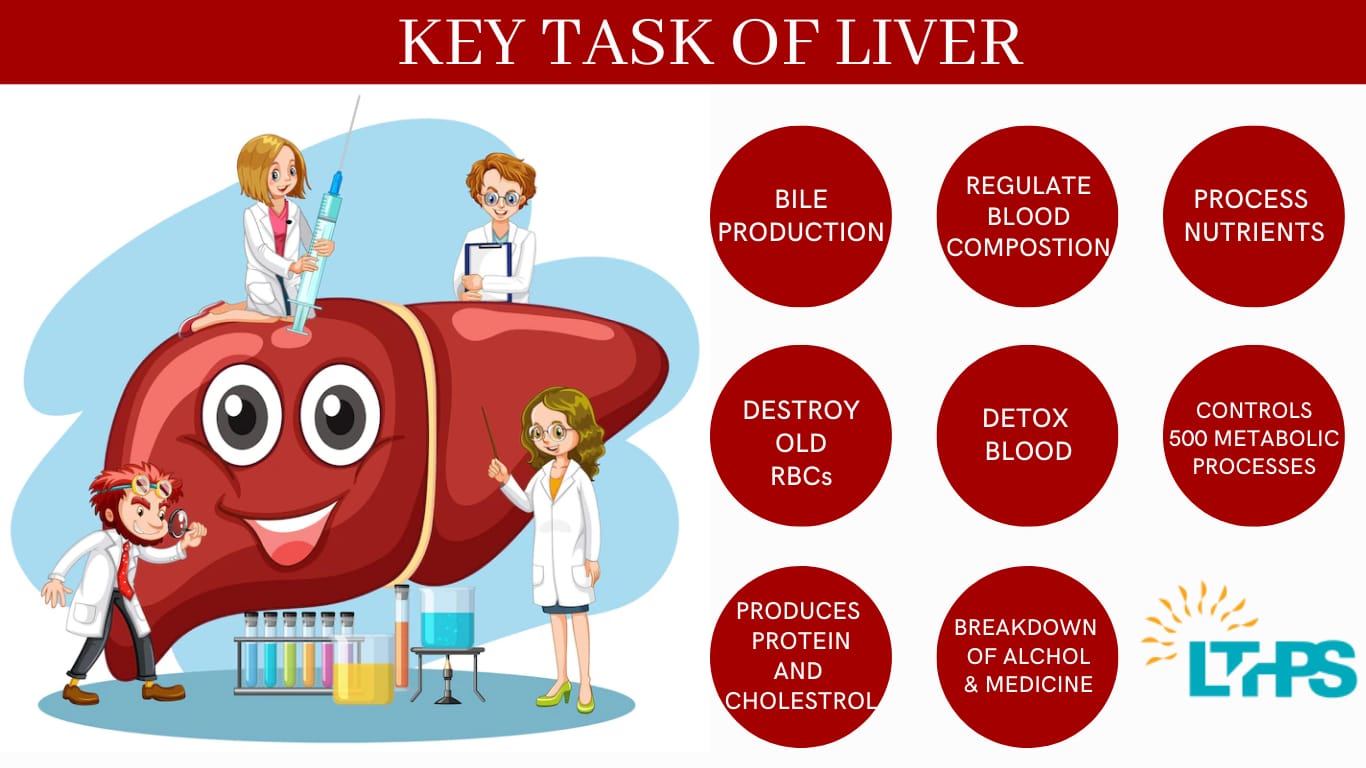
A dysfunctional liver has a significant effect on the rest of your body. The organ carries out hundreds of essential functions, from assisting with food digestion to removing dangerous toxins from your blood. You might need a liver transplant procedure to repair your failing liver if the problem is serious enough.
We have information for you if you want to learn more about liver transplants in India or why it’s the best country for foreigners. So let’s get this conversation started.
When Is A Liver Transplant Necessary?
There are numerous reasons for liver disease to be serious enough to necessitate a liver transplant. Cirrhosis is the most frequent cause of liver transplants in adults. In cirrhosis, a prolonged insult to the liver causes it to steadily degrade and malfunction. Scar tissue takes the place of healthy liver tissue, partially restricting blood flow through the liver. Drinking, autoimmune liver illnesses, fat deposits in the liver, genetic diseases, and viruses like hepatitis B and C can all lead to cirrhosis.
Many persons with liver cirrhosis from binge drinking also require a liver transplant. Some of them will often experience considerable improvements with alcohol abstinence and problem management for six months, and these individuals may live for extended periods without a transplant. Liver transplantation is the only option for people with severe liver disease when long-term abstinence and medical care don’t improve their health.
What Makes India the Best Country for Liver Transplant Surgery for Foreign people?
We all know that India is quickly becoming a center for medical tourism for all types of healthcare services, making it possible for many Indian hospitals to accept patients from throughout the globe. Indian hospitals are taking advantage of the chance to provide the best medical care for those in need.

A liver transplant in India has several wonderful advantages, including:
Affordability
India is primarily recognized for its accessibility. The rupee’s position on the international market is the main factor influencing India’s affordable healthcare. It has changed the liver transplantation trend in India. The best hospital and liver transplant facilities are less costly than any hospital or institution in other wealthy countries.
Knowledge and Experience of Indian Physicians
Patients from industrialized countries like the US, UK, France, etc., hold doctors from India in high regard. They meet the needs of individuals and are recognized as some of the best in the world.
Create Facilities of the Highest Quality
Indian hospitals are comparable to those in developed countries. They are expanding continuously to compete with hospitals from wealthy countries. As we all know, a liver transplant needs specialist equipment and is a highly technical surgery, both of which Indian hospitals can provide.
Use modern technology
The most modern Indian hospitals have their own research centers and equipment and constantly search for ways to enhance patient care. Moreover, Indian medical facilities use the most recent diagnostic and treatment equipment for liver transplants. They also have no concerns about using the newest liver transplantation innovation.
Conclusion
A liver transplant surgery removes a sick liver and implants a healthy one in its place. Around 38 years have passed since such operations began. Some liver transplant recipients go on to have completely normal lives.