Even while returning home following a liver transplant is a joyous occasion, a high level of worry may mark the initial weeks. Despite possible issues, most transplant patients resume their regular activities and habits within three months. They engage in employment, family life, child-rearing, community service, and leisure activities.
You may have to modify your food after a liver transplant to maintain the health and function of your liver and to avoid gaining too much weight. Maintaining a healthy weight can prevent infections, elevated blood pressure, and other problems.
You will collaborate with your nutritionist (dietitian) and other parts of your care team to develop a healthy eating strategy that suits your requirements and enhances your way of life.
Why is food safety crucial for someone who has had a liver transplant?
After a big procedure like a liver transplant, you’ll need to take immunosuppressive drugs for the rest of your life. You can avoid the dangers of organ rejection by taking these medications, but your body’s natural defenses will significantly weaken once you begin taking them. As a result, it is crucial to concentrate on the diet to replace all the minerals you have lost, support you as you adjust to the alterations, and deal with any post-surgical damage. As a result, you must concentrate on consuming healthy food and preparing it correctly.
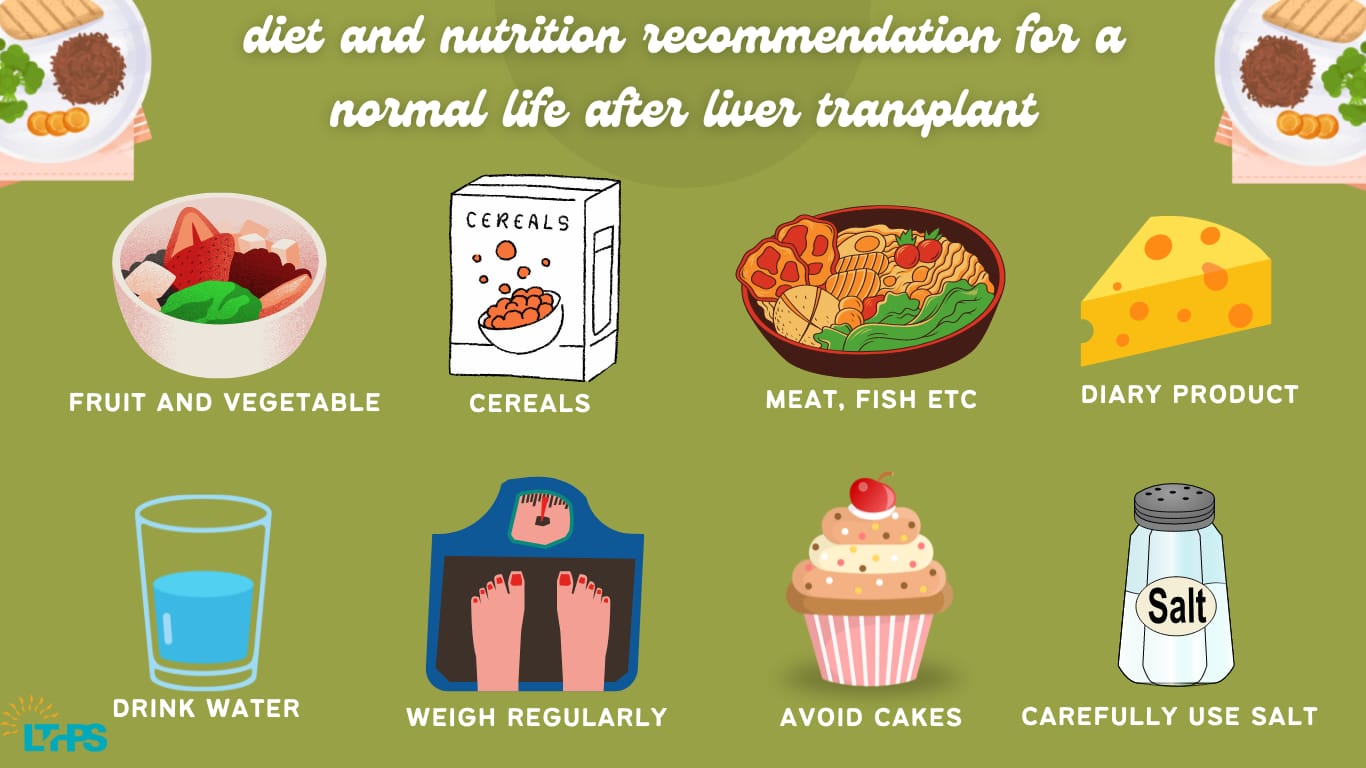
Diet and nutrition recommendations for a normal life after a transplant
Before the transplant, you were sick for a considerable time and likely lost significant weight. As a result, eating right is crucial to your healing process, and a good, balanced diet will assist in getting you back on track.
- Fruits and vegetables are an important part of your diet.
- Whole-grain baked goods and cereals
- Lean meats, fish, chicken, and other protein sources. Low-fat and dairy foods or other calcium-containing foods.
Additional Suggestions for Food After a Liver Transplant include:
- Weighing yourself daily.
- Steer clear of sugary snacks like cakes and cookies between meals. Consume some fruit or veggies if you’re hungry.
- Try to consume two liters of fluid daily. This benefits your kidneys and aids in the body’s elimination of waste. Fruit drinks, herbal beverages, pasteurized low-fat milk, and packaged mineral water are all healthy options.
- Peel and carefully wash fresh fruit.
- Potatoes and other vegetables cultivated in the soil must always be peeled and prepared in boiling water. Vitamin concentration in vegetables can be preserved by pressure cooking them. Consume no raw veggies, such as lettuce.
- Prevent cheeses with mold, and never eat cheese manufactured from unpasteurized milk.
- Purchase little quantities of dairy products frequently so you can consume them while they’re still fresh.
Salt (Sodium)
Use salt carefully while cooking, avoid salting cooked foods or salads, and steer clear of salty items like potato chips, pickles, and canned goods while using steroids.
Exercise
Following a daily workout regimen is crucial to strengthen your muscles after a protracted sickness has weakened them. You must increase the number of workouts you do slowly. Walking, swimming, biking, and improving your general muscle tone are all excellent ways to build stamina. If all goes well, you can start participating in other activities three months after the surgery. Never begin an exercise routine without first consulting your transplant team.
Driving
Driving a car is not advised for the first four weeks after liver transplantation. You should not consume alcoholic beverages. The liver breaks down alcohol, which can harm the liver.
Smoking
Give up smoking! Smoking is bad for your health in general.
Sexual Behavior
As soon as you feel healthy enough, you can start having sexual relations again. A few months following surgery, most men restore their sexual ability, while most women discover that the menstrual cycle has returned to normal.
Fertility
Many men have effectively fathered offspring following transplantation, and a sizable number of individuals have given birth to viable offspring. Women should talk to their physician or a transplant teammate about their desire to begin a family.
It would help if you typically waited at least one year before trying to conceive. You must also undergo low-dose immunosuppressive medication, have the good renal function, and be clear of any conditions that could compromise the health of you or your unborn child.
Vacation
If you apply common sense, there is no explanation for why you shouldn’t enjoy your travels. Always bring enough medicines with you for the duration of the trip. Always provide contact information, such as an address.
Household Pets
Having pets in the home is typically not advised due to the elevated risk of infection.
Protein
 Any competent and knowledgeable liver transplant specialist in a place with such modern medical technology would advise protein to make up one-fourth of the food for at least two months following the liver transplant as part of the rehabilitation program. You must have protein in your meals and beverages if you want long-term medical benefits. Lean meat, eggs, seafood, and chicken are also satisfying options for non-vegetarians. Vegans can benefit from soy milk, and vegetarians need not fear because dairy products, beans, and lentils are also excellent protein sources. In addition to this, nuts and seeds are sources of protein. A key piece of advice is to consume low-fat milk products to prevent weight gain.
Any competent and knowledgeable liver transplant specialist in a place with such modern medical technology would advise protein to make up one-fourth of the food for at least two months following the liver transplant as part of the rehabilitation program. You must have protein in your meals and beverages if you want long-term medical benefits. Lean meat, eggs, seafood, and chicken are also satisfying options for non-vegetarians. Vegans can benefit from soy milk, and vegetarians need not fear because dairy products, beans, and lentils are also excellent protein sources. In addition to this, nuts and seeds are sources of protein. A key piece of advice is to consume low-fat milk products to prevent weight gain.
Fats
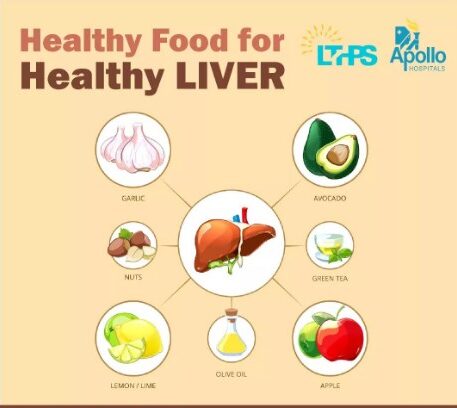
In addition to slowing recovery, a rise in bad cholesterol might result in other health issues. Healthy fats, however, can increase the positive effects on your health. Consume cold-water fish, like tuna. Omega 3 fatty acids, abundant in fish, are very good for your health. Nuts, vegetable oils, and seeds are excellent sources of good fats.
Conclusion
A sophisticated medical operation called a liver transplant includes replacing a patient’s diseased or non-functioning liver with a healthy part retrieved from a compatible donor. Patients with end-stage liver problems who are not reacting well to medicine or other treatments are advised to have an operation. It is crucial to watch your diet after a liver transplant because the liver is crucial to digestion. You need to pay close attention to what you eat and don’t consume, keep a healthy weight, and steer clear of any conditions that can harm your liver.