Have you ever felt a peculiar pain or fullness in your upper belly and thought if it is something to be worried about? Perhaps your physician insinuated liver enlargement, which has now left you with numerous questions. What is the reason? Is it life-threatening? Is treatment possible?
You are not the only one. Liver enlargement or hepatomegaly, as it is known in the medical field, can signal many things. But do not worry, in this guide, we will explain everything you need to know step by step in simple and relatable terms.
Let us start.
1. What is Liver Enlargement?
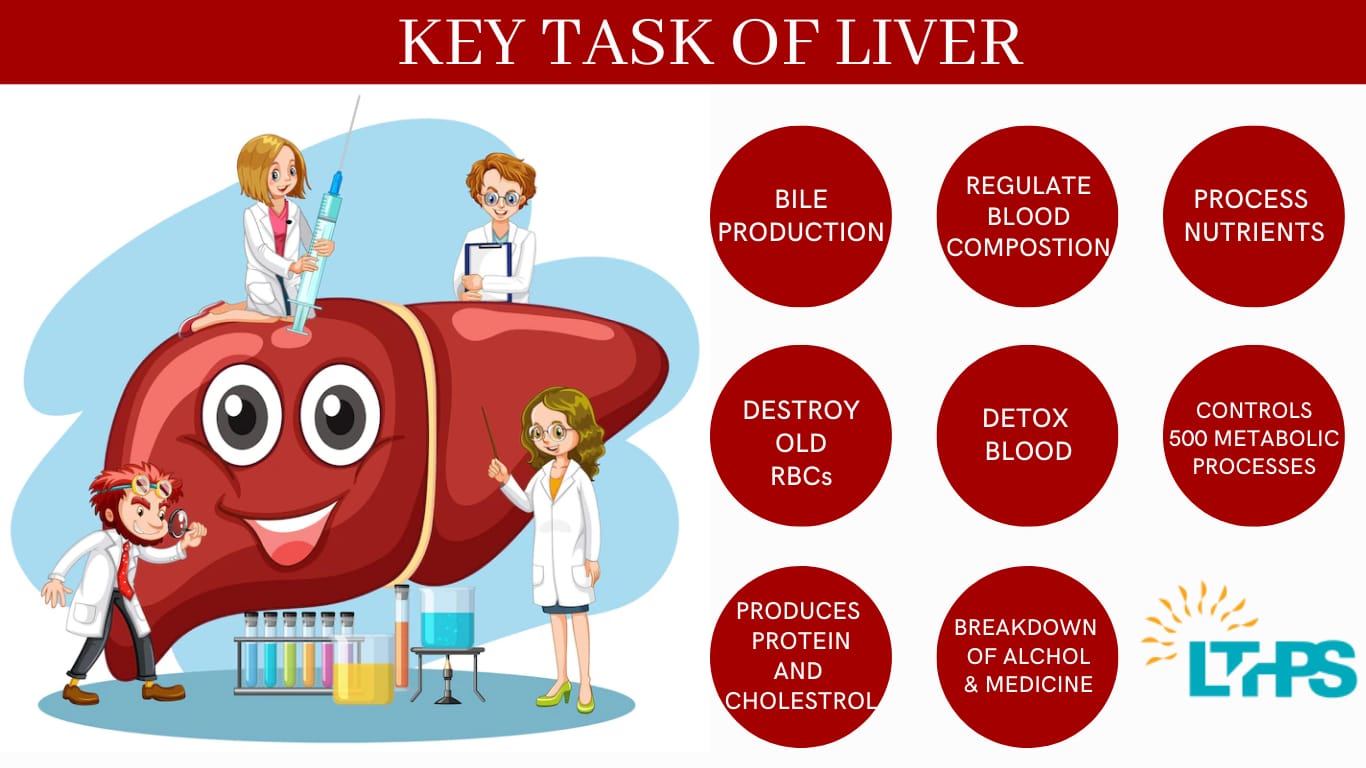
Your liver, which is about the size of a football, is situated just beneath the rib cage on the right side. Whenever it is enlarged, it indicates something is wrong. Conceptualise your liver as a sponge- it absorbs everything. If the sponge binds up too much, it begins to swell. This swelling may be mild and groundless or severe and painful.
2. What Causes Liver Enlargement?
There is no one answer to this. The causes of increasing the liver’s size, hepatomegaly, stem from a varied number such as fat accumulation to serious infections or malignant tumours. Some of the causes are soluble, while some may need to be controlled for a long time or even require surgery to replace the organ.
3. Fatty Liver Disease: A Silent Culprit
- Liver obesity is one of the most prevalent causes of liver swelling, especially among those who are overweight or diabetic. The gradual overaccumulation of fat in liver cells leads to inflammation and swelling.
- There are two forms:
- NAFLD (Non-Alcoholic Fatty Liver Disease) – Unrelated to alcohol consumption.
- AFLD (Alcoholic Fatty Liver Disease) – Results from excessive alcohol consumption.
- Most of the time, no symptoms are experienced until it progresses. This is why regular check-ups are important.
4. Alcohol-Related Liver Damage
Excessive consumption of alcohol leads to inflammation and swelling of liver cells. Recurrent damage increases the risk of developing cirrhosis. It is one of the top factors that leads to patients requiring a liver transplant.
5. Hepatitis Infections and Liver Inflammation
Hepatitis B and C are known for causing inflammation of the liver, and chronic infections tend to damage the liver over time without revealing the extent to which it is swollen and the problems it might cause.
Lack of treatment can result in liver failure or cancer, which makes the work of a specialist on transplants very important.
6. Liver Cancer and Tumours
Cancerous lesions on the liver can induce hepatomegaly. Whether the malignancy is primary or secondary, it is important to detect it early.
All tumours require investigation, and they may be benign or malignant.
7. Heart Conditions That Affect the Liver
Correlates with the previous one, as for some strange reason, it actually works the other way around. If your heart is not functioning properly, it can also lead to some backing of blood which results in swollen liver: also referred to as congestive hepatomegaly.
Most people suffering from heart failure or chronic heart disease often suffer from this condition.
8. Genetic and Metabolic Disorders
- These might also be inherited, such as:
- Liver Wilson’s Disease
- Hemochromatosis (excessive iron)
- Alpha-1 Antitrypsin Deficiency
- If these remain untreated, they can lead to long-term and progressive liver swelling.
9. Warning Signs and Symptoms
- Here’s what to look out for:
- A feeling of fullness or bloating
- Upper right side abdominal pain
- Jaundice
- Nausea and feeling exhausted
- Swelling in the legs or abdomen
- Patients may not detect the changes immediately, but if they persist, further investigation would prove valuable.
10. What Are the Steps Taken in Diagnosing Liver Swelling?
- In diagnosing liver swelling, doctors rely on a mix of:
– Through the physical examination
– Blood tests (including Liver function tests)
– Imaging techniques (Ultrasound, CT scan, MRI)
– In rare instances, a liver biopsy
All these contribute to determining the cause and degree of the problem.
11. Indicators for Consulting with a Liver Transplant Specialist
If the cause of swelling is severe liver disease or liver failure, it is best to consult a liver transplant specialist. They specialise in determining if there is any possibility of liver recovery or if a transplant is the sole option.
Usually, early detection of the disease can greatly reduce the chances of surgery.
12. Options Available for Treating a Swollen Liver
- The approach taken is determined by the liver problem in concern:
– Fatty liver – requires diet and exercise
– Hepatitis requires antiviral medications
– Alcoholic liver disease requires stopping alcohol consumption completely
– Tumours -require surgery, chemotherapy, and/ or radiation - In some scenarios, the liver can heal on its own if timely treatment is provided.
13. What Lifestyle Adjustments Can Support Your Liver?
- Think of your liver as an employee who always works overtime with no breaks. For that employee to continue working, they must be sustained. Here’s how:
– a. Nutrition – Reduce unhealthy meals, increase fruits and vegetables.
– b. Physical activity – Exercise helps lower fat deposits.
– c. Alcohol consumption – Reduce intake or stop altogether.
– d. Unnecessary medication usage – Avoid it.
Even the smallest of changes can contribute to a positive difference.
14. Indicators for Consideration of a Liver Transplant
- Repeated infections as well as irreversible liver damage are marked by the following:
- Recurrent liver failures
- Cancerous growths in the liver
- Cirrhosis of the liver grade 3, painless.
- Advanced complex form,s eg, bleeding complications or deep coma.
- Here, looking for the Best Liver Surgeon in India becomes critical to one’s life situation.
15. The Best Liver Surgeon in India
The country is swiftly emerging as a one-stop shop for advanced-level liver treatment. The Best Liver Transplant Surgeon in India are not only highly trained, but they also work in first-class hospitals with modern equipment and have great outcomes.
In this case, best means:
- Experience and specialisation
- Public opinion/ reviews about patients
- Facilities/ level of the hospital
- Care after surgery
- Given the choice of a pilot for a hard flight, you want the best hands to hold the controls of the aeroplane.
Final comments:
Liver inflammation is either a warning or, with more serious complications down the line, your body is saying, “there is more to this.”
Your liver works hard, especially when it comes to processing toxins, so make sure to give it some TLC.
FAQs
1. How likely is it for a swollen liver to return to its original size?
As long as the underlying reason is managed and treated, like through lifestyle modifications or medication, the liver is often able to return to its normal size.
2. Which foods should be avoided to prevent swollen livers?
These individuals should avoid repugnant foods, such as alcohol, fried foods, processed sugars, red meat. These individuals should focus on vegetables, whole grains, lean meats, and proteins.
3. How long does it take for a liver to heal?
It can take weeks to months to recover depending on how well one is managing the condition. Those with more advanced conditions may take longer.
4. What type of X-rays are used for the swelling of the liver?
Examples of liver function tests include ultrasounds and MRIs. These are commonly used for liver functions.
5. Which doctor has the most experience in liver transplant surgeries in India?
Every primary hospital will have highly qualified experts. The patients should look for doctors that have high patient ratings and comments.
| Dr. Neerav Goyal as a liver transplant specialist: |
| To seek a consultation with a best liver transplant doctor in New Delhi , India: |
| Call us at 8527516541 | Email at [email protected] |