Have you ever wondered how your liver silently keeps you healthy every single day? Think of it as your body’s personal “detox factory” — working tirelessly to filter toxins, digest fats, and store energy. But what happens when this hardworking organ starts to fail?
Liver damage often creeps in quietly, showing signs that are easy to overlook. By the time symptoms become noticeable, significant damage may have already occurred. Recognizing these early warnings can make all the difference between timely treatment and serious complications.
In this article, we’ll explore the five major signs of liver damage, their causes, and when to seek help from a liver transplant specialist in India.
Table of Contents
| Sr# | Headings |
|---|---|
| 1 | What Does the Liver Do? |
| 2 | Why Liver Damage Happens |
| 3 | Sign #1: Constant Fatigue and Weakness |
| 4 | Sign #2: Yellowing of Skin and Eyes (Jaundice) |
| 5 | Sign #3: Swelling in the Abdomen and Legs |
| 6 | Sign #4: Dark Urine and Pale Stool |
| 7 | Sign #5: Itchy Skin and Easy Bruising |
| 8 | Additional Signs You Should Watch Out For |
| 9 | How Is Liver Damage Diagnosed? |
| 10 | Early Treatment and Lifestyle Management |
| 11 | When to Visit a Liver Transplant Specialist in India |
| 12 | Importance of Timely Medical Attention |
| 13 | Preventing Liver Damage – Everyday Tips |
| 14 | Foods That Help Heal the Liver Naturally |
| 15 | Conclusion |
1. What Does the Liver Do?
Your liver is one of the busiest organs in your body. It performs over 500 essential functions, including:
- Filtering toxins from the blood
- Producing bile to aid digestion
- Regulating blood sugar levels
- Storing vitamins and minerals
- Breaking down alcohol and medications
- In short, your liver acts like your body’s “chemical factory”, constantly processing and filtering everything you eat, drink, and absorb.
2. Why Liver Damage Happens
Liver damage can result from many factors, including:
- Excessive alcohol consumption
- Fatty liver disease (both alcoholic and non-alcoholic types).
- Viral hepatitis (Hepatitis A, B, or C).
- Obesity or diabetes.
- Certain medications and toxins.
When your liver is overloaded or inflamed, it starts to lose its ability to function properly. Over time, this can lead to liver cirrhosis, liver failure, or even the need for a liver transplant.
3. Sign # 1: Constant Fatigue and Weakness.
Feeling tired all the time– even after resting? Persistent fatigue is often one of the earliest signs of liver damage.
When your liver can’t effectively filter toxins, they start accumulating in your bloodstream. This can make you feel sluggish, foggy, or exhausted without a clear reason.
Tip: If tiredness lingers for weeks, accompanied by loss of appetite or mild nausea, don’t ignore it. A simple blood test can help detect early liver issues.
4. Sign # 2: Yellowing of Skin and Eyes (Jaundice).
Jaundice is a classic symptom of liver trouble. It causes your skin, eyes, and even nails to turn yellow due to the buildup of bilirubin– a yellow pigment produced during the breakdown of red blood cells.
A healthy liver processes bilirubin efficiently, but when damaged, this process slows down, leading to visible yellowing.
Watch out for:.
- Yellow-tinted skin or eyes.
- Dark urine and pale stools.
- Itching.
If you notice these changes, it’s crucial to consult a liver transplant specialist in India for evaluation and treatment.
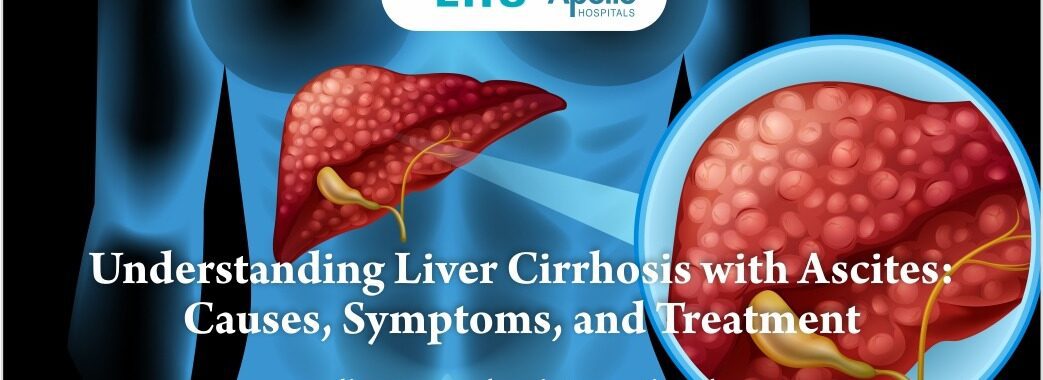
5. Sign # 3: Swelling in the Abdomen and Legs.
If your stomach feels bloated or your legs appear puffy, it could be fluid buildup due to poor liver function. This condition is called ascites (in the abdomen) and edema (in the legs).
The liver produces proteins that help maintain fluid balance in the bloodstream. When it fails, fluid leaks into surrounding tissues, causing visible swelling.
- Seek help immediately if you experience:.
- A tight or bloated belly.
- Rapid weight gain.
- Difficulty breathing due to abdominal pressure.
This is often a sign of advanced liver disease requiring urgent attention.
6. Sign # 4: Dark Urine and Pale Stool.
Changes in urine and stool color can reveal a lot about your liver’s health.
Dark urine (tea or cola-colored) indicates excess bilirubin.
Pale or clay-colored stool suggests that bile isn’t reaching the intestines properly.
Together, these are telltale signs that your liver or bile ducts are not functioning as they should.
7. Sign # 5: Itchy Skin and Easy Bruising.
Ever noticed unexplained itching or bruising? Damaged livers struggle to produce clotting proteins, making bruises appear easily.
Itching, on the other hand, occurs due to bile salts accumulating in the skin, which irritates nerve endings.
In short:.
When your skin starts talking, your liver might be crying for help.
8. Additional Signs You Should Watch Out For.
- Apart from the five major signs, other subtle symptoms of liver damage include:.
- Nausea or vomiting.
- Loss of appetite.
- Unintentional weight loss.
- Confusion or memory problems (hepatic encephalopathy).
- Bad breath or metallic taste.
While these may seem harmless, they can point to ongoing liver inflammation.
9. How Is Liver Damage Diagnosed?
- Diagnosing liver damage involves a combination of tests, including:.
- Liver function tests (LFTs): Measure enzyme and protein levels.
- Ultrasound or MRI: Detects fatty changes or tumors.
- Liver biopsy: Confirms the extent of damage.
A liver transplant specialist in India may also recommend additional imaging or viral screening to determine the cause.
10. Early Treatment and Lifestyle Management.
If detected early, liver damage is often reversible with proper care.
Lifestyle tips:.
Avoid alcohol completely.
Eat a liver-friendly diet rich in fruits, veggies, and whole grains.
Maintain a healthy weight.
Get vaccinated against hepatitis A and B.
Avoid unnecessary medications and herbal supplements.
11. When to Visit a Liver Transplant Specialist in India.
You should consult a liver transplant specialist in India if:.
Your doctor detects cirrhosis or liver failure.
Your symptoms don’t improve despite lifestyle changes.
You have a known liver condition like hepatitis or fatty liver.
Specialists not only manage advanced liver disease but also guide you through transplant options if needed, ensuring the best possible outcome.
12. Importance of Timely Medical Attention.
Delaying treatment can allow liver damage to progress silently into irreversible failure. Remember, the liver has an incredible capacity to heal– but only if given a chance.
Ignoring early signs is like ignoring warning lights on your car’s dashboard. The sooner you act, the better your chances of recovery.
13. Preventing Liver Damage– Everyday Tips.
Stay hydrated.
Limit processed and fried foods.
Exercise regularly.
Get routine liver function tests, especially if you have diabetes or obesity.
Simple daily choices can protect your liver from long-term harm.
14. Foods That Help Heal the Liver Naturally.
Include these in your diet for a healthier liver:.
- Garlic– aids detoxification.
- Turmeric– reduces inflammation.
- Green tea– rich in antioxidants.
- Leafy greens– help flush toxins.
- Coffee– surprisingly beneficial in moderation.
These foods support liver repair and overall health.
15. Conclusion.
Your liver is the ultimate multitasker– working day and night to keep you alive and well. The signs of liver damage often start small, but early recognition can save your life.
If you notice persistent fatigue, yellowing of the eyes, or swelling, don’t ignore them. Consult a liver transplant specialist in India for expert diagnosis and guidance.
Caring for your liver today ensures a healthier, happier tomorrow.
FAQs.
1. What are the early signs of liver damage?
Early signs include fatigue, yellowing of the eyes (jaundice), dark urine, and mild abdominal swelling.
2. Can liver damage be reversed?
Yes, if caught early and the cause is removed– such as stopping alcohol or treating hepatitis.
3. When should I see a liver transplant specialist in India?
If you have cirrhosis, severe symptoms, or poor liver test results, consult a specialist immediately.
4. What foods are good for liver health?
Garlic, turmeric, green tea, and leafy greens support detoxification and repair.
5. Is liver transplant the only option for severe liver damage?
Not always. Early medical management can stabilize the liver, but advanced cases may require a transplant.