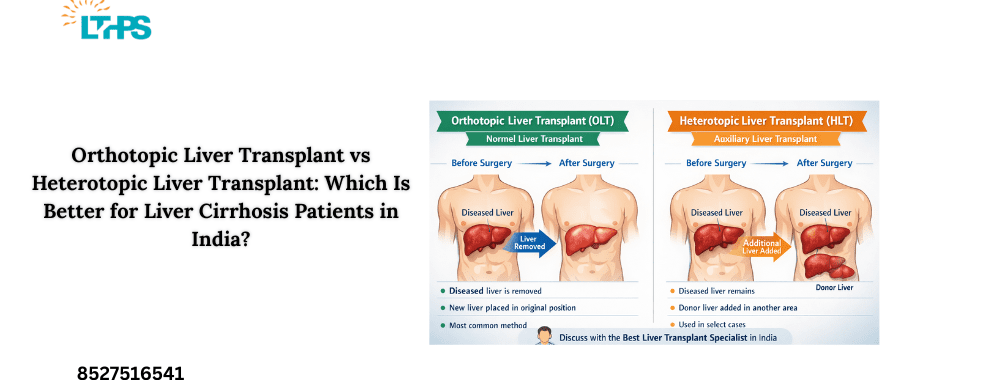
Liver cirrhosis is a serious health condition that affects many people in India. When the liver stops working well, doctors may recommend a liver transplant. But did you know there are different kinds of liver transplants? The two main types are Orthotopic Liver Transplant (OLT) and Heterotopic Liver Transplant (HLT). In this blog post, we’ll explain both in simple terms and help you understand which one might be better for cirrhosis patients in India.
We will also talk about when to call your doctor and give a clear summary at the end. This post uses easy language so liver patients and caregivers can understand their options. If you or a loved one is dealing with liver disease, this article can help you make informed decisions with your healthcare team, including the best liver transplant surgeon in India or the best liver transplant specialist near you.
Introduction
Liver cirrhosis happens when healthy liver tissue is replaced by scar tissue. This makes it hard for the liver to work properly. Over time, cirrhosis can lead to liver failure. When medicines and lifestyle changes are not enough, a liver transplant may be the best option.
Two transplant methods exist:
Orthotopic Liver Transplant (OLT)– the diseased liver is removed and a new liver is placed in the same spot.
Heterotopic Liver Transplant (HLT)– the patient keeps their old liver, and a new liver is placed in a different location inside the body.
This article explains both types, compares them, and gives helpful information for patients in India.
What Is an Orthotopic Liver Transplant (OLT)?
Before Surgery After Surgery
—————- —————-
[ Diseased Liver ] —> [ Healthy Donor Liver ]
| |
Removed Replaced
👉 Key idea:
The damaged liver is completely removed, and the donor liver takes its place. This is the most common and preferred method for liver cirrhosis patients.
In Orthotopic Liver Transplant (OLT), the surgeon removes the diseased liver and replaces it with a healthy donor liver in the exact position.
Key Points About OLT
- The diseased liver is taken out completely.
- The new liver goes in the original liver’s place.
- This is the most common type of liver transplant worldwide.
Why OLT Is Common
It gives the patient a fresh, healthy liver with full function.
- Surgeons are very experienced with this method.
- Many studies show that long-term survival rates are higher with OLT
- Pros of OLT
- Better long-term results for many patients.
- Less risk of the patient’s old liver causing problems later.
- The new liver works where it is meant to work.
- Cons of OLT.
It is a big surgery and may take longer.
Recovery may take more time at first.
Doctors often recommend OLT to patients with advanced cirrhosis because it gives them the best chance to live longer and healthier.
What Is a Heterotopic Liver Transplant (HLT)?
In Heterotopic Liver Transplant (HLT), the patient keeps their original liver and the new donor liver is placed in a different part of the abdomen.
Before Surgery After Surgery
—————- —————-
[ Diseased Liver ] —> [ Diseased Liver ]
+
[ Donor Liver ]
(Placed in another area)
👉 Key idea:
The patient keeps their original liver, and a second liver is added to help support liver function. This is rarely done and used only in special cases.
Key Points About HLT
The old liver stays inside the body.
A second liver is added and works alongside the diseased one.
- This type is less common.
- Why HLT Is Used
- HLT may be an option when:
- The patient can not tolerate a long surgery.
- There is a need to support liver function for a short time.
- Surgeons want to give the patient extra liver help without removing the old liver.
- Pros of HLT
- Surgery may be shorter.
The patient’s own liver remains undisturbed.
It may be helpful in specific medical situations where full liver removal is risky.
Cons of HLT
The old liver can still cause problems.
Space inside the abdomen is limited.
It may not work as well in the long term as OLT.
HLT is rare and only used in certain cases. Many liver experts view it as a backup or supportive transplant rather than a first choice.
Comparing OLT and HLT: What’s the Difference?
To make a good decision, it helps to see how both options compare.
- FeatureOrthotopic Liver Transplant (OLT) Heterotopic Liver Transplant (HLT).
Removes diseased liver ✔ ❌.
Places new liver in original spot ✔ ❌.
Surgery lengthLongerShorter.
Long-term successHighModerate.
Use in cirrhosisStandard choiceRarely used.
ComplexityHigherLower in some cases.
In simple terms:.
OLT replaces the sick liver with a new one in the same place.
HLT adds another liver without removing the old one.
For most liver cirrhosis cases, especially in India, OLT is the standard and more reliable option when a patient is fit for surgery and a suitable donor liver is available.
Which Is Better for Liver Cirrhosis Patients in India?
Both types have benefits, but for liver cirrhosis patients, doctors most often recommend Orthotopic Liver Transplant (OLT). Here’s why:.
1. Better Long-Term Outcomes.
OLT gives a complete replacement of the diseased liver. This means:.
Less scar tissue left behind.
Better liver function over time.
Lower chance of future liver problems.
Many medical reports and patient studies have shown that people who receive OLT tend to live longer and have better quality of life.
2. More Experience in India.
Surgeons in major Indian cities like Delhi, Mumbai, Chennai, and Hyderabad have more experience with OLT. This includes best liver transplant surgeon in India specialists who perform these surgeries regularly.
3. Lower Risk of Complications.
HLT leaves the diseased liver in place, which can still cause portal hypertension and other problems. With OLT, the old liver is removed, and the body only relies on the healthy donor liver.
4. Better for Advanced Cirrhosis.
In advanced liver cirrhosis, the liver is badly damaged and scarred. Leaving it inside may not help the body much. Replacing it with a healthy liver, as done in OLT, gives patients a stronger chance at recovery.
Who Is a Good Candidate for OLT vs. HLT?
Good Candidates for OLT.
Patients who:.
Have advanced liver cirrhosis.
Have good heart and lung health.
Can withstand a major surgery.
Have a matching donor liver available.
Patients for Whom HLT Might Be Considered.
HLT is rare but might be considered when:.
The patient has specific surgical risks.
Shorter surgery time is critical due to health issues.
HLT can act as temporary support until a full transplant is possible.
However, most liver specialists in India still prefer OLT when possible.
Risks and Benefits at a Glance.
Benefits of OLT.
Replaces the damaged liver completely.
Better long-term survival.
Reduces future liver-related complications.
Most widely used method.
Risks of OLT.
Major surgery with longer anesthesia.
Risk of infection or bleeding.
Requires lifelong follow-up and medication.
Benefits of HLT.
Shorter surgery.
Might help patients who can’t tolerate full transplant.
Risks of HLT.
Diseased liver still present.
May not support full recovery.
Less common, fewer long-term studies.
Life After Liver Transplant.
Whether you receive OLT or HLT, life after surgery requires care and commitment:.
Follow your doctor’s instructions.
Take anti-rejection medicines every day.
Eat a balanced diet.
Avoid alcohol.
Get regular check-ups.
Watch for signs of infection or complications.
Patients need strong support from family and healthcare teams, including the Best Liver Transplant Specialist to guide them through recovery.
When to Call Your Doctor.
It’s important to know when to seek help. Call your doctor right away if you notice:.
- High fever (above 101 ° F).
- Severe pain in the belly.
- Yellow skin or eyes (jaundice).
- Confusion or extreme tiredness.
- Swelling of legs or belly.
- Unusual bleeding or bruising.
- Redness or discharge from wound sites.
These can be signs of complications that need urgent medical attention.
5-Point Summary.
Here’s a quick recap:.
OLT replaces the diseased liver, while HLT adds a second liver.
OLT is the standard and preferred choice for most liver cirrhosis patients in India.
HLT is rare and used only in special cases.
Long-term results are generally better with OLT.
Always consult a best liver transplant surgeon in India or Best Liver Transplant Specialist for personalised care.
Pre-Transplant Care: Preparing for a Liver Transplant
Getting ready for a liver transplant is just as important as the surgery itself. Proper pre-transplant care improves success rates and helps the body handle surgery better.
1. Medical Evaluation and Tests
Before listing a patient for transplant, doctors perform several tests, including:
Blood tests to check liver function
Imaging tests like ultrasound or CT scan
Heart and lung fitness tests
Infection screening
These tests help the Best Liver Transplant Specialist decide if the patient is fit for surgery.
2. Managing Liver Cirrhosis Symptoms
While waiting for transplant, doctors focus on controlling symptoms such as:
Fluid buildup in the abdomen (ascites).
Confusion or memory problems.
Fatigue and weakness.
Bleeding risks.
Medicines, diet changes, and regular monitoring are very important during this phase.
3. Nutrition Before Transplant.
Good nutrition helps the body stay strong:.
Eat high-protein foods unless advised otherwise.
Reduce salt to prevent swelling.
Avoid raw or unhygienic food.
Stay well hydrated.
Malnutrition is common in cirrhosis patients and must be corrected before surgery.
4. Avoid Alcohol and Smoking.
Complete alcohol avoidance is mandatory. Even small amounts can disqualify a patient from transplant eligibility. Smoking should also be stopped to reduce lung and heart risks.
5. Mental and Emotional Preparation.
A liver transplant can feel overwhelming. Counseling helps patients and families:.
Understand the procedure.
Prepare mentally for surgery.
Learn about lifestyle changes.
Support from family plays a big role in transplant success.
Post-Transplant Care: Life After Liver Transplant.
Life after a liver transplant requires long-term care and commitment. With proper follow-up, most patients enjoy a healthy and active life.
1. Hospital Recovery Phase.
After surgery:.
Patients stay in ICU for monitoring.
Vital signs and liver function are checked closely.
Pain control and infection prevention are priorities.
Hospital stay usually lasts 2– 3 weeks, depending on recovery speed.
2. Lifelong Medications.
After transplant, patients must take:.
Anti-rejection medicines daily.
Antibiotics or antivirals (initially).
Supplements as advised.
Skipping medicines can cause organ rejection, which is why guidance from the best liver transplant surgeon in india is crucial.
3. Diet and Lifestyle After Transplant.
Healthy habits protect the new liver:.
Eat balanced, home-cooked meals.
Avoid raw food and street food.
Maintain a healthy weight.
Drink clean, safe water.
Alcohol should be strictly avoided even after transplant.
4. Regular Follow-Ups and Tests.
Post-transplant care includes:.
Frequent blood tests initially.
Gradual spacing of doctor visits.
Monitoring for infection or rejection.
Early detection of problems ensures better long-term outcomes.
5. Preventing Infections.
Because anti-rejection medicines lower immunity:.
Avoid crowded places initially.
Maintain good hygiene.
Report fever or illness immediately.
Simple precautions can prevent serious infections.
6. Emotional Health and Quality of Life.
Mood changes, anxiety, or stress may occur after transplant. Patients are encouraged to:.
Speak openly with doctors.
Join support groups.
Stay active physically and socially.
Most patients return to work and normal life within a few months.
Key Takeaway for Patients.
✔ Proper pre-transplant care improves surgery success.
✔ Strict post-transplant discipline protects the new liver.
✔ Guidance from the Best Liver Transplant Specialist is essential.
✔ Lifestyle changes are lifelong– but rewarding.
Conclusion.
Choosing between an orthotopic liver transplant and a heterotopic liver transplant is not simple. For most liver cirrhosis patients in India, Orthotopic Liver Transplant (OLT) remains the better choice because it offers more long-term benefits. However, every patient is different. The final decision should be made with the help of an experienced liver transplant team, including the best liver transplant surgeon in India you can trust.
Taking time to understand your options can help you make better decisions for your health. If you have more questions about liver transplant types or need support, don’t hesitate to talk with your healthcare provider.
Frequently Asked Questions (FAQs).
1. Which liver transplant is better for liver cirrhosis patients in India?
For most patients with liver cirrhosis, Orthotopic Liver Transplant (OLT) is considered better because it completely replaces the damaged liver and offers better long-term results.
2. Why is Heterotopic Liver Transplant rarely done in India?
HLT is rarely done because:.
The diseased liver remains inside the body.
Long-term results are not as strong as OLT.
Most Indian transplant centers specialize in OLT.
That’s why the best liver transplant surgeon in india usually recommends OLT.
3. Is Orthotopic Liver Transplant safe?
Yes. When performed by an experienced team and Best Liver Transplant Specialist, OLT is a well-established and safe procedure with good survival rates.
4. Can a patient live a normal life after liver transplant?
Yes. Many patients return to a near-normal life after transplant by:.
Taking medicines regularly.
Avoiding alcohol.
Eating healthy food.
Attending follow-up visits.
5. How do I choose the best liver transplant specialist?
You should look for:.
Experience in liver transplants.
High success rates.
Multidisciplinary transplant team.
Hospital with ICU and transplant facilities.
Consulting the best liver transplant surgeon in india ensures proper guidance and long-term care.
6. When should a cirrhosis patient consider liver transplant?
A liver transplant should be considered when:.
Medicines stop working.
Frequent fluid buildup occurs.
Confusion (hepatic encephalopathy) develops.
Repeated hospital admissions happen.
Early consultation with a Best Liver Transplant Specialist improves outcomes.